INDICATIONS FOR SURGICAL TREATMENT IN HAMSTRING TEARS AND HAMSTRING SYNDROME
Lasse Lempainen
Hospital Mehiläinen NEO, Turku, Finland
Introduction
Most hamstring injuries are treated conservatively with good results. However, there are cases in which surgery should be considered already in the acute phase. Also there are cases in which surgery should be considered later if non-operative treatment appears to be unsuccesful.
Terminology
Nomenclature of the injury should be muscle / tendon specific. Concerning injury classification, the term ’partial tear’ comprising collectively all the three hamstring muscles is nowadays not accurate enough. Instead of talking about a partial hamstring tear we should talk about a partial biceps femoris (BF) tear, for example. Furthermore, more information would be obtained if isolated muscle/tendon ruptures were categorized also proximally as complete ones (grade III injury), for example, complete proximal semimembranosus (SM) rupture. Also the location of the tear is of importance. A proximal avulsion is often treated differently than a tear in the muscular part.
A term ’central tendon’ has been suggested regarding injuries in the muscular part where then tendon is surrounded by the muscle belly. The term has been applied also in other than hamstring injuries, e.g. in the rectus femoris.
Absolute indications for surgery
In an athlete a proximal one tendon avulsion with clear retraction should be treated surgically regardless of the hamstring tendon (BF, SM or ST). If two or all three of the hamstring muscles are avulsed surgery should be considered in all patients if there are not major contraindications to surgery. Suture anchors are typically used to reattach the tendon to bone (Figures 1 and 2).
Apophyseal avulsions of the ischial tuberosity occur occasionally in adolescent athletes. Surgical repair is traditionally recommended if the avulsed fragment is displaced by more than 10-15 mm (Figures 3 and 4).
Distal tears of the hamstrings are rare. The BF is most commonly affected and most of the tears are incomplete. The BF or the semitendinosus (ST) may, however, rupture completely from the distal bony insertion or at the distal myotendinous junction. An acute complete rupture (BF or ST) with a retraction should be repaired anatomically. It is important to note that the behaviour of an acute distal ST avulsion is not similar to that of harvesting the tendon for graft purposes like in ACL reconstructions. In surgery typically a debridement and suturing is done and sometimes in distal tears the ST is attached to the SM if continuity cannot be restored anatomically.
Relative indications for surgery
Occasionally incomplete tears especially when recurrent form scar tissue and adhesions that cause persistent symptoms and are non-responsive to conservative treatment. This can occur in the proximal or distal bone-tendon interface or in the proximal or distal tendinous part or in the paramuscular area. In proximal incomplete avulsions that remain symptomatic the MRI may show liquid between the bone and the tendon which is a sign of incomplete healing.
It has been suggested that central tendon injuries especially in the BF may have a higher risk of poor healing with conservative treatment. Also the risk of a recurrent injury may be high. In these injuries there is often an incomplete tear of the paramuscular tendon typically in the area of 5 to 20 cm from the proximal origin (Figures 5, 6 and 7). Often the muscle tissue is torn off from the tendon also. When a tear like this remains symptomatic after adequate conservative treatment or there are recurrences surgery should be considered. Full continuity of the central tendon is restored with sutures and the attachment of the muscle to the tendon is reinforced. It is important to avoid overthightening of the repaired tendon. Scar tissue may be removed. Suture anchors may be used if the tear is located close to the bony origin.
Chronic injuries
In chronic proximal hamstring ruptures and in some rerupture cases, anatomic apposition of the retracted muscles cannot always be achieved. In those cases fascia lata autograft augmentation can be used to connect the retracted hamstrings to ischial tuberosity. It seems that late reconstruction of complete proximal hamstring avulsion with fascia lata autograft augmentation results in enhancement of muscle strength, better function of the hamstrings and improved the leg control. Also symptoms derived from retracted hamstrings causing stretching to the sciatic nerve could be alleviated.
Hamstring Syndrome
Proximal hamstring tendinopathy, also reported under the name of hamstring syndrome, is supposedly an overuse injury which expresses itself by lower gluteal pain especially during sports and also often while sitting. It has been seen in athletes of various sports activities but especially in sprinters and middle- and long-distance runners. Chronic hamstring syndrome can be very resistant for conservative treatment and surgery may be indicated. In hamstring syndrome partial tenotomy of the semimembranosus tendon and exploration of the sciatic nerve is a valuable option and it yields highly successful return to sports in most cases.
Conclusions
Even though surgery is rarely necessary for hamstring muscle injuries, it has an important role in treatment of the most severe cases. In fact, its role may even increase in the future. In my experience, hamstring injury severity is often underestimated, and clear surgical cases – such as when the proximal tendon is retracted distally from the anatomical footprint – are often missed. This has serious consequences for the recovery time and functional outcomes, which are of upmost importance to the athlete.
When choosing a treatment method,it should be remembered that hamstring injuries can be career ending injury. Surgical treatment should always be considered when athletes sustain complete proximal or distal tendon avulsions. Finally, it is important to note that surgery is technically easier if performed soon after the injury has occurred.
Figures 1-2. Complete proximal biceps femoris and semitendinosus rupture at the left side.
- Figures 1-2. Complete proximal biceps femoris and semitendinosus rupture at the left side.
- Figures 1-2. Complete proximal biceps femoris and semitendinosus rupture at the left side.
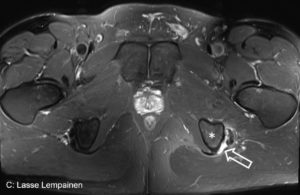
Figures 3-4. Avulsion fracture with clear retraction at the right side.
- Figure 3
- Figure 4
Figures 5-7. Central tendon rupture of the biceps femoris with clear retraction. Peroperative view before and after repair.
- Figure 5
- Figure 6
- Figure 7